Cervical cancer
Female, 46 years, poorly differentiated squamous cell carcinoma 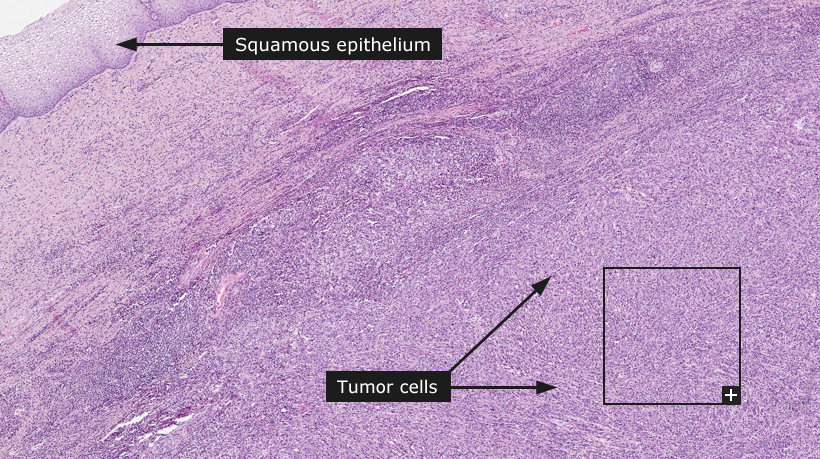
Cervical cancer
The cervix is the narrow, lower portion of the uterus that joins the top of the vagina with the uterine body. Cervical cancer is the third most common type of cancer in women worldwide. One of the most common symptoms of cervical cancer is abnormal vaginal bleeding, but in some cases there may be no obvious symptoms until the cancer is in its advanced stages.
Cervical cancer usually develops very slowly, often over a period of months and years. It initially forms as a precancerous condition called dysplasia. This precancerous condition can be detected by a Pap smear (a cytology specimen retrieved from the cervix for microscopical examination) and is completely treatable. Most women who are diagnosed with cervical cancer today have not had regular Pap smears or they have not followed up on abnormal Pap smear results. The widespread use of cervical screening programs has reduced the incidence of invasive cervical cancer by 50% or more in countries with successful screening programs. However, Pap smear screening remains a challenge in developing countries such as India and China. Consequently, the incidence of cervical cancer in these countries is high.
The Human Papilloma Virus (HPV), that can spread through sexual intercourse, is the cause of nearly all cervical cancers. There are many different types of HPV and certain strains lead to high risk for developing cervical cancer. Risk factors include having sex at an early age, multiple sexual partners, smoking and poor socio-economic status.
Cervical cancers arise from cells in the transitional zone of the cervix. The transitional zone is the border between squamous epithelium, that cover the lower portion of cervix (ectocervix) and the columnar, glandular cells that line the endocervical channel. Most cervical cancers originate from cells that show squamous differentiation and are hence squamous cell carcinomas. Cancers arising from the columnar cells are defined as adenocarcinomas and are more rare.
The FIGO (International Federation of Gynecology and Obstetrics) staging system recognizes four stages of cervical cancer. Stage I depicts cancer limited to the cervix. Stage II denotes cervical cancer that has spread beyond the cervix but not to the lower third of the vagina or the pelvic wall. Stage III cancers have spread to the pelvic wall and/or lower third of the vagina. Stage IV tumors extend beyond the true pelvis or clinically involve the mucosa of the bladder and/or rectum. With treatment, 80 to 90% of women with stage I cancer and 50 to 65% with stage II cancer are alive 5 years after diagnosis. Only 25 to 35% of women with stage III cancer and 15% or fewer of those with stage IV cancer are alive after 5 years.
A vaccine to prevent cervical cancer is now available. In June 2006, the U.S. Food and Drug Administration approved a vaccine which prevents infection by the two types of high-risk HPV responsible for most cervical cancers. Studies have shown that the vaccine appears to prevent precancerous lesions and early-stage cervical cancer.
Normal tissue: Cervix, uterine
|