Testis cancer
Male, 32 years, mixed germinal cell tumor, dominating yolk sac component 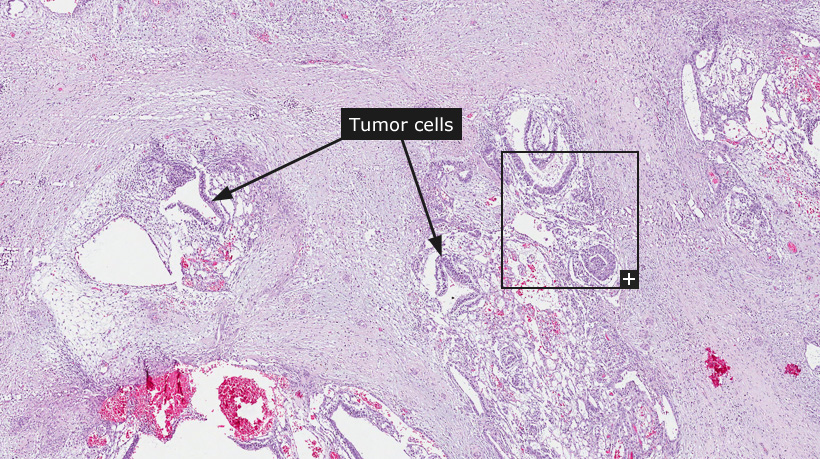
Testis cancer
Testicular cancer constitutes approximately 1% of cancer in males. Tumors of germ cell origin account for approximately 95% of all testicular cancers. Clinical pathology plays a key role in management of patients with testicular tumors as it allows for accurate classification of tumors and thus to facilitate decisions regarding treatment and follow-up. Microscopic evaluation aids to identify the histological type, determine the extent of tumor growth in surrounding tissues and to confirm the absence or presence of invasion into the vascular and/or lymphatic system.
Testicular cancer is divided into two major categories: seminoma and non-seminomatous germ cell tumors. Non-seminomatous tumors are further classified as pure or mixed tumors. Tumors containing both seminomatous and non-seminomatous components are regarded as non-seminomatous germ cell tumors for treatment purposes.
Seminomas account for approximately 45% of all germ cell tumors and are characterized by evenly spaced and relatively large uniform tumor cells with distinct cell borders. Tumor cell nuclei are often centrally localized and show distinct nuclear membranes and one or two distinct nucleoli. The characteristic tumor stroma in seminoma is built up by a delicate fibrovascular network with thin collagenous septa containing variable amounts of small lymphocytes.
Of the non-seminomatous tumors, embryonal carcinoma accounts for 15-30% and represents the second most frequent pure type of testicular cancer. Embryonal cancer shows an acinar, tubular, papillary or solid growth pattern with areas of necrosis, hemorrhage and fibrosis. Tumor cells are highly pleomorphic with large, irregular nuclei and indistinct cell borders. Embryonal carcinoma is a relatively undifferentiated germ cell tumor from which the other more differentiated components are derived. These non-seminomatous components include 1) endodermal sinus tumor (yolk sac tumor), typically characterized by the presence of Schiller-Duval bodies (resembling a central capillary lined by flattened layers of tumor cells), and 2) choriocarcinoma, representing extra-embryonic development, and 3) teratoma, representing embryonic development. Teratomas can in turn be composed of both immature and mature components representing cell types and structures from all embryonic germ layers.
The distinction between different tumor types and components within a testicular tumor is based on microscopical examination and in addition to morphology, immunohistochemistry provides important information. Commonly used antibodies for the differential diagnostics of these tumors include D2-40, OCT 3/4, hCG and AFP in addition to CD30 (TNFRSF8) and markers of intermediate filaments, e.g. cytokeratin (KRT) and vimentin (VIM).
Schiller-Duval bodies are said to resemble a glomerulus. They have a mesodermal core with a central capillary, all lined by flattened layers of both visceral and parietal cells.
Normal tissue: Testis
|